Traumatic Brain Injury
Early Platelet Dysfunction Following Traumatic Brain Injury
In the United States alone, 52,000 deaths occur due to traumatic brain injury (TBI). As a result of TBI, there are 275,000 hospitalizations and 1.365 million emergency department visits per year. TBI is a contributing factor to a third of all injury-related deaths in the US.
Acute coagulopathy is a serious complication of TBI, and is of uncertain etiology due to the complex nature of TBI. However, recent work has shown a correlation between mortality and abnormal hemostasis due to early platelet dysfunction. The goal of the current study is to develop and characterize a rodent model of TBI that mimics the human coagulopathic condition, so that mechanisms of the early acute coagulopathy in patients with TBI can be more readily assessed. Studies in rats demonstrate a strong correlation with important post-injury pathological changes that are observed in human TBI patients, viz., diminished platelet responses to agonists, especially ADP, while platelet counts remain in normal ranges, and subarachnoid bleeding. Additionally, administration of a direct thrombin inhibitor, pre-injury, recovers platelet functionality to ADP stimulation, indicating a direct role for excess thrombin production in TBI-induced early platelet dysfunction.
Currently, collaborative efforts between the W.M. Keck Center and Memorial Hospital are in the process of correlating observations from the rodent model and human TBI patients. Both human and rodent samples are being used to further our understanding of the mechanisms of platelet dysfunction. The clear dysfunction of ADP-induced platelet activation in severe head trauma patients has led to a greater defined clinical point-of-care approach. This has enabled physicians at Memorial Hospital to improve patient prognoses both short and long term.
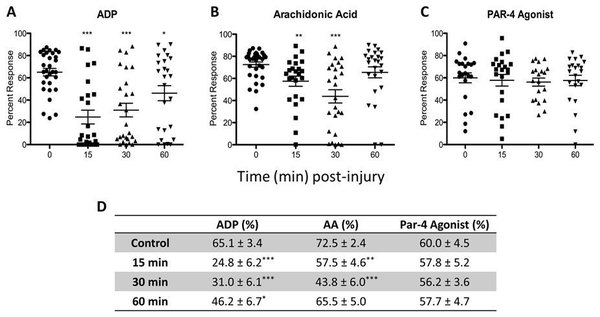
Platelet mapping expressed as percent platelet response induced by (A) ADP; (B) AA; (C) P AR-4 agonist; (D) summarized values. Statistical analysis was performed using an unpaired t-test by comparing a specific post-injury time to the control.
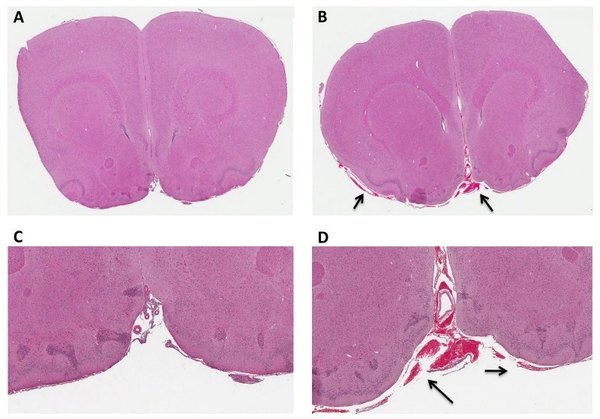
Subarachnoid blood pools 1 hr post-injury in TBI-induced rats. Representative 4 ìm coronal sections of control (A,C) and 1 hr post-injury (B,D) rat brains. Arrows indicate bleeding in the subarachnoid space of the injured brain. Images were scanned at 40X magnification and zoom magnified at 1.2X for A, B and 4.5X for C, D.